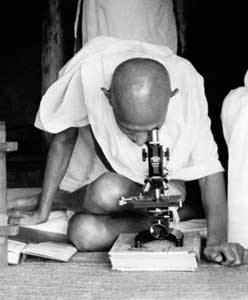
[Picture from the website of Theodore Gray, who had what looks like a great day with Oliver Sacks.]
Is a doctor a consultant, giving her patients advice about how to select medical interventions (or avoid them) based on her understanding of her patient's values? Or is she something else--something more complicated, and emotional?
I was thinking about this after part of a small discussion/debate with one of my favorite teachers, someone who makes it a big part of her job to be extremely thoughtful about the doctor-patient relationship. In my thesis (which I defended yesterday), I cited Robert Rimer, a person with AIDS who wrote a book called "HIV+: Working The System" in 1993, who describes a doctor as being a consultant to the patient; she was responding to this theme with both agreement and skepticism.
But I was thinking about the conversation later in part because I misunderstood part of one of the questions my teacher was asking in our conversation. In retrospect, I think she was arguing that part of what a doctor is supposed to do is care, not just in the sense of providing medical care, but also building an emotional connection and a sense of emotional investment that both the doctor and the patient feel. I agree that this is an important–and extremely rewarding–part of the doctor's job. But when she said, "You describe this as a very intellectual kind of relationship" I agreed with that too.
I'd like to think that part of how I care for people is to be their expert, to be the dork that works for them, their personal geek. And I'm skeptical about the people who dwell too much on the theme of "humanism in medicine", which I think more often than not is just the latest medical buzz phrase for common decency–and yet another chance to pat ourselves on the back. I think doctors are supposed to be decent human beings who treat their patients with respect and concern, but I don't think that's any special calling or anything unique to medicine. I think it's a basic rule of human interaction in an egalitarian society.
Of course, when we are talking with our doctors about really serious parts of our lives, we need to believe that they care about the content of our conversation. And I admit that there is a unique kind of vulnerability that we have with our doctors. Often we are talking with doctors about our own physical frailty, our mortality, and the private intimacies of bodily sensations, bad smells, and objectionable substances. These are things we go to great lengths to hide under all other circumstances.
And so there is also a special emotional obligation on doctors to honor and attend to that vulnerability. And it's true that this is where the "consultant" metaphor begins to break down a little. This vulnerability, not to mention social class, social convention, and even the architecture of the exam room, all conspire to create a real power difference between patient and doctor that is not quite like a classic consulting relationship.
This is not some corporate CEO calling in some Harvard kid who works for McKinsey, to ask how to improve web site traffic.
The emotional currents that run between doctor and patient make a kind of live wire. Those currents can be exploited on both ends. Doctors get a lot of training (especially informal training, which often reinforces some bad values) on how to prevent getting used and manipulated by people who are walking into the clinic or the hospital with a set of agendas that doctors don't want to serve. Psychiatrists spend a lot of time talking to each other about monitoring their own emotions during sessions as a way of using their own emotional state as a kind of sensor to help them understand what the patient is going through. For instance, if psychiatrists start to feel agitated and confused during a visit, if they can stand back from that sensation for a moment they can recognize what it is about the patient (usually agitation and confusion) that is triggering this feeling.
But most patients walk in without that kind of tool. When the electricity of powerful emotions begins in the exam room, they're caught without gloves on. This sometimes clouds people's thinking and makes it difficult to contrast their own agendas with the doctor's agenda. When this happens, it's not until later, when they've left the exam room and gone home, and the electrical current fades and then shuts off, that they realize that they wanted something different from this visit than the doctor did. In other words, I think sometimes people can sink into the emotional connection they get from the clinic–which can be powerful–and lose the ability to clearly and precisely advocate for themselves.
So when I talk about being a consultant, it is not with the aim of eliminating emotion from the exam room, nor with the aim of failing to care for the patient. But that care has to give some breathing room; it can't be enveloping, or it will suffocate the patient's own power and initiative, or constrain its birth and growth.
Anatole Broyard wrote:
"My ideal doctor would be my Virgil, leading me through my purgatory or inferno, pointing out the sights as we go. He would resemble Oliver Sacks, the neurologist who wrote Awakenings and The Man Who Mistook His Wife for a Hat. I can imagine Dr. Sacks entering my condition, looking around at it from the inside like a benevolent landlord with a tenant, trying to see how he could make the premises more livable for me. He would see the genius of my illness. He would mingle his daemon with mine: we would wrestle with my fate together."
This is a complicated, even jumbled, set of metaphors. But the ideas are useful, and not just because they're about Oliver Sacks. Broyard describes the doctor first as a guide; and then, as a kind of owner of one's own condition, a guide who can not only show you around but help improve the premises.
In this way of describing the doctor, the doctor is important because of his expertise; but also because he employs that expertise with kindness. It's important here to note that Oliver Sacks as a man is actually frankly odd, or so it seems from his lovely book Oaxaca Journal. In the book he takes a tour of Oaxaca with a group of fern aficionados; he is also a quite dedicated fern aficionado. He often sets himself apart from the group, most of whom are paired off in couples. He is clearly the nerd, and the striking thing about this, of course, is that he is the nerd among a group of people who have devoted a considerable amount of their free time to thinking about ferns.
Nonetheless, after a while, he begins to become engaged in some mild running jokes with a couple of his fellow travelers, and to build relationships in a way that seems totally ordinary to me as a reader. (He seems to be thrilled by one of his dorky running jokes, even perhaps by the very idea of a running joke. I have this kind of running joke with various people in my world all the time, as do most of you, dear readers.) And yet by the end of his trip he feels completely happy in a way that he rarely has before.
He writes:
"I myself may be the only single person here, but I have been single, a singleton, all my life. Yet here this does not matter in the least, either. I have a strong feeling of being one of the group, of belonging, of communal affection–a feeling that is extremely rare in my life, and may be in part a cause of a strange "symptom" that I have had, an odd feeling in the last day or so, which I was hard put to diagnose, and first ascribed to the altitude. It was, I suddenly realized, a feeling of joy, a feeling so unusual I was slow to recognize it. There are many causes for this joyousness, I suspect–the plants, the ruins, the people of Oaxaca–but the sense of this sweet community, belonging, is surely a part of it."
I believe, reading Oliver Sacks, that he must be a good doctor. Clearly Anatole Broyard believed the same thing. And yet if we are to believe his journal it seems to take him completely by surprise to feel a sense of belonging among other human beings, and that only transiently. How can this be if the essence of being a good doctor is human connection?
There are a couple of possible answers. One is that Oliver Sacks is a wonderful writer but a lousy doctor. It's hard to know if this is true, but even harder to believe. Another is that Oliver Sacks feels as if he is not making human connections even when he is. This seems more likely.
Most of all, Oaxaca Journal made me think that Oliver Sacks has a sense of solidarity with his patients in the neurology clinic, in the sense that he is acutely and intuitively aware of the idea of neurodiversity. However it is that his brain works, he is quite aware that it is not like other peoples' brains. And when Temple Grandin described herself as "an anthropologist on Mars", and he titled his book of essays with this phrase, it's hard not to wonder whether Sacks himself does not feel sometimes like an anthropologist on Mars, albeit a very kind and enthusiastic anthropologist.
But we know for sure that Oliver Sacks is driven by fascination, by intellectual interest in people and how they think and how they perceive the world. He is able to be fascinated in a kind way, and his fascination is infused by solidarity. And this is what is moving and wonderful about his writing. I think this is also what probably makes him a good doctor, and a good consultant.
He is not taking you out of hell, though if he can walk you towards the door out, he will. He is showing you around, and explaining what is going on there, and working with you to see if things can be better if this turns out to be where you are going to have to live. Anatole Broyard and I read Oliver Sacks and see this in him, and we think that this seems like what a doctor is supposed to be.
I hope to do the same for my patients: to be kindly fascinated, to feel a sense of solidarity with them, and help show them around. Is this caring? Sort of; in fact, it can even feel like a kind of love. But not exactly. It is not a parental or even a fraternal kind of love; it is not even friendship, really.
When we are ill, and live in fogs of pain or nausea or fear of death, it is the people who love us who should love us, and hold us, and remind us of what is good about the fact that we lived on this world and breathed its air. Doctors can do this in a pinch; but so too can many other people. Most people think their nurses are actually better at it.
So what's the point of a doctor? What's the doctor supposed to be? The answer is somewhere in this area of metaphors, of consultants and guides. The point of the doctor is to illuminate the inner landscape and history of our own bodies, to show us around when it becomes confusing, to suggest a way out when we get lost, or a way to get comfortable if we are trapped.
If I did not believe deeply in the value of that expertise, and if I only wanted to be kind and concretely useful to people who were suffering, I would have been a nurse, or perhaps a hospice volunteer. I actually spent a lot of time thinking about this choice, and it was not an easy one for me. But to become a doctor, I needed to accept the idea that I am not first a carer. I am a guide, who cares.