This post has been modified since its original posting. See end of post.
When I was choosing a residency, I decided to choose one where HIV care was part of their primary care program, supported by specialists, rather than exclusively part of a specialty clinic. This factor was actually far and away the biggest determinant of my choice, and I think studying the history of AIDS was part of what convinced me of the importance of the distinction.
Over the long run, scientists who worked on antiretrovirals to target HIV's replication were correct in their ultimate goals. It's this strain of HIV research and clinical strategy that gave us Highly Active Antiretroviral Therapy (HAART). And HAART dramatically increased survival times. But for a long time, antiretroviral
drugs were actually accomplishing little other than temporary improvements in immune cell counts.
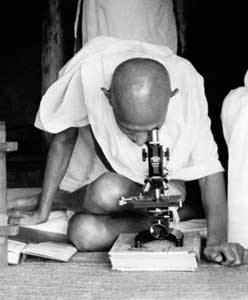
Until 1996, the biggest gains were made in thinking about how to better prevent and treat opportunistic infections and other problems of HIV and AIDS. Paradoxically, for some time, it was doctors like Joseph Sonnabend and activists like Michael Callen (the picture above is of Callen), who did not believe that HIV caused AIDS, who probably provided some of the best clinical advice for most of the 1980s.
For people who were focused on the virus, it seemed like madness to avoid a drug like AZT when it first came out. It had demonstrated activity against the virus and people who took it often had rises in their CD4 counts (the cell marker that serves as a main indicator of immune health in people living with HIV). But AZT gave people sometimes severe anemia, as well as other problems like sometimes intolerable nausea. That was especially true at the high doses which AZT partisans initially recommended. Worst of all, it turned out that giving AZT alone really didn't give a clear survival advantage. (The debate about how much time it bought for some people, and at what cost, was never really resolved.)
In other words, in the 1980s, people like Sonnabend and Callen were scientifically wrong, but clinically right. And people who emphasized antivirals over all else – pushing high-dose AZT and not attending aggressively enough to opportunistic infections and other issues of immune well-being – were scientifically right, at least in the narrow sense, but clinically wrong.
The people who thought about AIDS research in a hyper-reductionist way did later win big gains for people with AIDS. In fact, they eventually transformed the epidemic. (Sonnabend now presecribes HAART and concedes the point of HIV's importance.)
But in the meantime, until 1996 or so, I think people with AIDS were probably usually served best by clinicians who started from observable clinical problems (opportunistic infections, immune collapse, and the personal issues that made it difficult for people to care for their health) and worked their way in. That was different from clinicians who started with the virus and worked their way out. Starting from observable clinical problems yielded better results than focusing on a theoretical model of the disease and treating the clinical problems as mere signals and stages of that model.
And that's despite the fact that the theoretical model was essentially correct.
At the triumphalist moment of the world AIDS conference in Vancouver in 1996, protease inhibitor maven Dr. David Ho started a presentation with the slide "It's the virus, stupid." This was the picture of a previously-frustrated reductionist slam-dunking his opponents. Ho had actually told Science reporter Jon Cohen that he was making a button with this slogan in 1993, but Vancouver was the moment of victory.
At the Vancouver conference, after a decade of developing antiretroviral drugs with essentially no impact on survival time, the virologists could finally claim the unequivocal success they'd been waiting for. The skeptics of the Callen and Sonnabend school finally had to admit that there was a direct relationship between the virus and the disease. (Denialists of the Duesberg school and its like have never been swayed by evidence, and the mounting evidence that proves them wrong has only made them stronger.)
But if Ho and other virologists were right about the value of targeting the virus from a variety of angles through combination therapy, they were wrong about what the target of AIDS therapy should be.
The point of HIV medicine is not HIV. The point of HIV medicine is people living with HIV.
On first blush that sounds like one of those cloying "humanism in medicine" truisms. But I've started thinking it's worth stating, forcefully.
I thought a lot about this when I was interviewing for a residency spot in internal medicine. I'm planning to be a primary care doctor with an emphasis on HIV. That's a different path than many HIV doctors take these days, particularly in my city, where an academic specialist-driven model is more prominent. (This really varies city-by-city, depending on what powerful people got behind which model.)
I still may end up getting training as an infectious disease specialist just because it will be practical to do so: to get the HIV training, I'll spend a year doing general hospital ID, doing consults on surgical wound infections, even knowing that this part of the specialty has almost nothing to do with HIV care.
There are also year-long HIV fellowships which train especially for HIV care; that's a more likely path for me. HIV medicine is not for the faint-of-heart; it's technically tough and full of insider jargon, so it's worth thinking of it as a specialized area of knowledge. But is that specialized area of medicine really more related to surgical wound infections than it is to heroin addiction, liver failure and vascular disease? I think it's not, and that's why I've chosen to think of HIV medicine, and my training for it, as part of primary care, not as a branch of infectious diseases.
In fact, we might ask: is the virus actually the biggest problem of people with HIV these days? In the United States, the phenomenal success of the HIV reductionists has created its own problems. People with HIV are starting to have cardiovascular and metabolic complications which are often still poorly understood. Some are the result of living for a long time with the virus itself. Others are the result of taking anti-HIV medicines for a long time.
It's not clear how much this will contribute to problems like heart attacks and stroke and diabetes, but a lot of folks think these will be bigger problems for people with HIV in the coming years. Plus, some of the people most at risk for HIV – people of color in poor neighborhoods – are also independently at higher risk for problems like diabetes and vascular disease, as well as other problems like addiction, social disruption and violence.
People with HIV still have all the challenges of taking medicines every day that they've always had. It's difficult for anyone to pull it off, no matter what their social circumstances. Addiction and poverty bring extra barriers. And for immigrants, language and discriminatory health access policies often make taking control of one's own medical care more difficult. The people who are hit hardest by the HIV epidemic in the United States are often people who also have significant problems other than HIV. And no matter how snazzy a doctor gets in prescribing drug combinations to get around the latest resistance mutation, the person living with HIV is the one who has to take the medicine every day.
In other words, many of the toughest challenges for people with HIV are once again challenges that are only indirectly related to the virus itself. These are primary care problems: How do people make their medical regimens a part of their lives? How do people reduce their risk for chronic problems like diabetes? How do you balance the benefit of medicines for one problem, versus the other problems they create? (And for that matter, one might very well ask, how can people with HIV live happy lives that are not entirely dominated by health concerns? but that is another story.)
The fact that infectious disease specialists are often the doctors responsible for HIV care is not inevitable. In fact, at the beginning of the epidemic, many ID doctors shied away from AIDS, as did many academic medical centers. The most academic of academic medical centers often avoided taking on much AIDS care in the early days of the epidemic. Their ID departments focused on other things. Perhaps coincidentally, but probably not, when big money started flowing in for AIDS research, they all started taking the epidemic seriously – hiring researchers and building up more serious clinical programs. But this approach didn't take the agendas of people with HIV as a starting point. It was built around the idea that AIDS was a problem caused by a virus, and that specialists in infectious agents should be the ones who provided HIV care.
There is an important difference in how different doctors think about the goal of HIV care. I think that a primary care model of HIV care is important not just because it's nicer or more medical-humanities-groovy; it's important because it is targeting the issues that are actually most clearly facing people with HIV. How do I live with these medications? How do I keep taking them? how do I live with the side effects? And how do I take care of my health beyond HIV? The success of the antiviral agenda has created a situation where we can generally take it for granted that we can knock down the virus that replicates inside people, but only if the person with the virus is able to commit to the effort to treat it, and only if other things don't kill that person first.
In other words, David Ho was wrong: It's the person, stupid.
Two post-scripts: I should add that even from the basic science point of view, the idea that "it's the virus, stupid" is disputed by HIV researchers who look at AIDS from the immune system's point of view. They point out that immune damage associated with HIV infection is partly caused by the immune response to the virus itself, and that the specific interaction of virus and immune system is more important than simply how much virus is present. See this paper and this erudite old-style medical journal commentary for more from the immunologists.
The second post-script: Looking at retrospective data for survival time it appears that using one antiretroviral like AZT in the late 1980s did not do anything for survival, but using two in people who had not taken one of them before did lengthen survival time somewhat. So, in hindsight, Callen and Sonnabend's particular kind of advice may have been less effective starting at some point in the early-to-mid-1990s, before 1996, when other drugs like AZT came out and could be used in combination with AZT.